2023-07-11 2272
4.2 Postoperative laser physiotherapy
Cefazoline for 7 days by subcutaneous injection twice a day, 25mg per kg. Meloxicam for 5 days by subcutaneous injection once a day, 0.1mg per kg. Laser treatment was added to the postoperative care, continuously for the first three days and once other day, three days later. On the 10th postoperative day, the pet was discharged.For 20 days after the operation, the pet owner reported that the pet did not have any abnormal phenomenon during the rest at home, and had good weight-bearing ability.
Laser treatment every other day during the first ten days of the postoperative recovery period can significantly improve the recovery rate of the affected limb and help the affected limb to recover its weight bearing quickly. In addition, laser treatment can better control pain, reduce the interest of incision after pet licking, and effectively reduce the probability of wound complications. Using TPLO surgery and laser treatment, patients with canine anterior cruciate ligament rupture have a 99% chance of successful treatment without any minor or major complications, and return to full function more quickly.
The precautions for adding postoperative laser therapy are as follows:
Treatment range: After TPLO, laser treatment should be used in a larger area, including the surgical incision, the entire knee, the muscle tissue associated with the knee, and the vasculature around the knee.
Procedure: The laser therapist will use the treatment head for contact irradiation around the surgical incision and gently massage to facilitate photon penetration into the tissue, using non-contact irradiation for the surgical incision.
Treatment cycle: one laser treatment should be performed 24 hours after TPLO. Laser treatment should subsequently be performed daily or other day, with the primary goal to help reduce postoperative swelling and edema following closure of the subcutaneous tissue and medial skin. Normally, from the second visit, we do not see any edema at the affected limb. When the patient reaches the expected recovery state, the laser treatment can be stopped, usually on day 10 after surgery. Unless we were dissatisfied with the treatment outcome, in this case, we continued the treatment twice weekly until a recovery of the affected pet was observed.
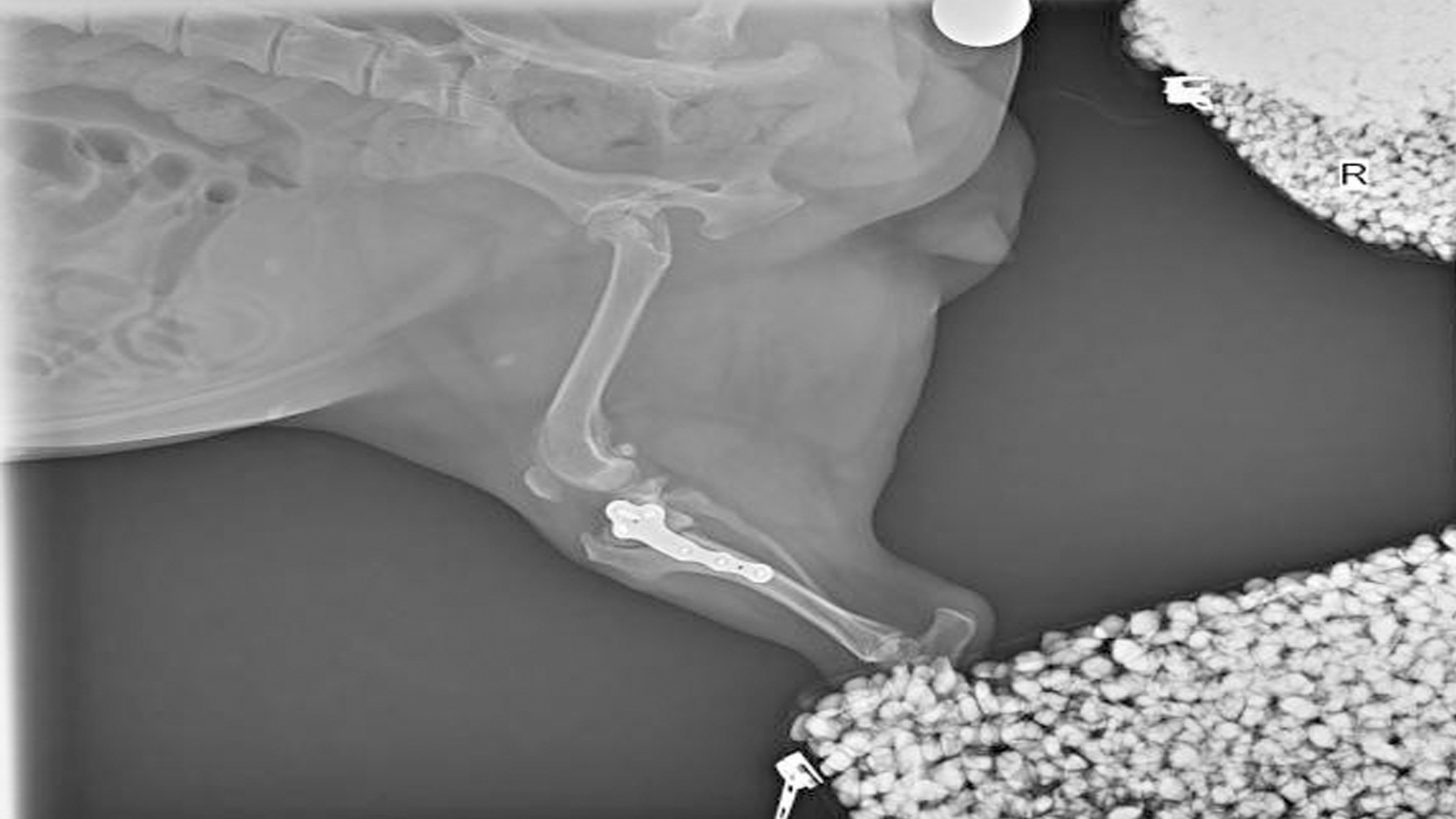
| Patients were reviewed one month and three months after surgery | |
 |
 |
 |
 |
| TPLO bones have healed and JOJO life returns to normal | |
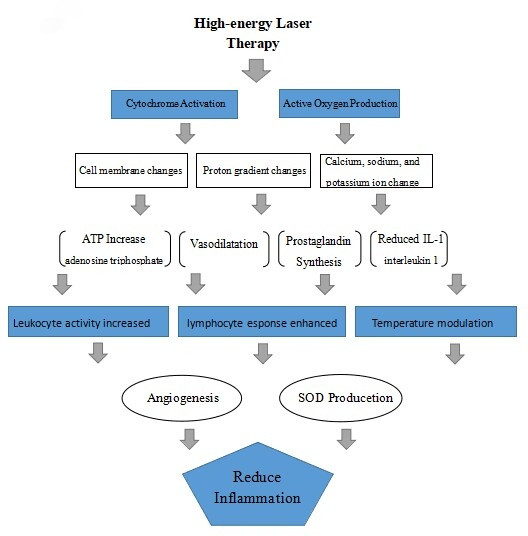
5.1 Laser irradiation can promote the reactive oxygen species (ROS) to regulate the intracellular Ca + + concentration, improve the Ca + + uptake in mitochondria, thus regulating the stability of the cell membrane.
Laser irradiation can promote the production of cytochrome c oxidase, which stimulates the generation and synthesis of adenosine triphosphate (ATP). ATP production and synthesis are significantly enhanced and contribute to cellular repair, propagation and functional capacity.
Laser irradiation can promote the increase of histamine, nitric oxide (NO) and serotonin, stimulate vasodilation, enhance the transport of nutrients and oxygen to damaged cells, and promote the repair and removal of cell debris.
Laser irradiation accelerates leukocyte activity, leading to an enhanced ability of noninactive cellular and tissue components to more rapidly repair and regenerate the function of damaged sites in the body.
Laser irradiation can increase prostaglandin synthesis, and PGI 2 (prostacyclin) has vasodilatatory and anti-inflammatory effects, with some properties similar to Cox-I and Cox-II inhibitors.
Laser therapy was able to reduce interleukin 1 (IL-1). Laser irradiation has a reducing effect on such proinflammatory cytokines implicated in the pathogenesis of rheumatoid arthritis and other inflammatory diseases.
In addition to increasing the number of lymphocytes, laser irradiation also mediates the role of lymphoid helper T cells and inhibitory T cells in the inflammatory response.
The laser-induced increase in NO and cell factor INF-g helps capillaries and lymphatic capillaries to increase and regenerate, thereby promoting blood circulation in the body and enhancing all repair and healing processes.
Inflammatory areas usually exhibit elevated temperatures. Laser therapy has been shown to accelerate body temperature normalization, demonstrating its beneficial effects on the inflammatory process.
Laser stimulates increased levels of cell factor superoxide dismutase (SOD) and interacts with other anti-inflammatory processes to accelerate the termination of the inflammatory process. The interaction between superoxide dismutase (SOD) and reactive oxygen species (ROS) production after laser treatment balances the free radical activity and allows reactive oxygen species (ROS) to exert beneficial effects.
Laser therapy has been shown to reduce the levels of inflammatory markers such as C-reactive protein and neopterin, especially in patients with rheumatoid arthritis.
The lower figure shows the summary flow chart of the cellular cascade to reduce tissue inflammation. The cumulative effects of these multiple interaction processes and events are accelerated inflammatory circulation, symptom reduction and early normalization.
5.2 The mechanism of laser treatment for painful diseases
High-energy laser can directly stimulate the release of endogenous endorphin and enkephalin through the use of biological stimulation and mechanical stimulation, thus inhibiting the conduction of A δ and C fibers. According to the pain gate control mechanism, the mechanical stimulation of free nerve endings leads to the inhibition of pain conduction, thus relieving the pain.
Irradiation of a high-energy laser can regulate the content of the serotonin (also known as serotonin hydroxytryptamine/5-HT). Serotonin is a neurotransmitter, serotonin-binding receptor (5-HT 3) and sensitized nociceptors, and antagonists of peripheral serotonin receptors (5-HT 2 A and 5-HT 3) that reduce pain produced by tissues.
Irradiation of a high-energy laser can reduce bradykinin. Bradykinin is an important cytokine capable of mediating inflammatory effects, which acts on nociceptors to cause pain and plays an important role in mediating inflammatory pain. Bradykinin has a wide range of functions, which can sensitize neurons, especially in the process of nociception. Inflammatory pain, rheumatoid pain, and pain sensation triggered by hypoxia are all accompanied by increased bradykinin concentrations. Therefore, the reduction of bradykinin can effectively relieve tissue pain.
Irradiation of a high-energy laser can modulate the function of acetylcholine. Acetylcholine is an excitatory transmitter with two different effects due to the presence of two different acetylcholinergic receptors, both excitatory and inhibitory. Adjust the function of acetylcholine receptor by irradiation laser, achieve the inhibition of nerve excitation and vasodilation to increase blood circulation, and produce the effect of relieving pain.
Through high-energy laser irradiation of the sympathetic ganglia in the affected area can cause blood flow increase, improve local blood circulation, improve cell metabolism level, promote peripheral circulation and lymphatic detoxification in the focal area, combined with biological stimulation effect and photochemical effect, and provide non-addictive pain management while promoting tissue healing.
High-energy lasers can also reduce the pain of wound stimulation. Laser irradiation can promote more oxygen atoms to reach the mitochondria, while promoting the terminal enzyme cytochrome C oxidase of the cell respiratory chain to accelerate the production of ATP, thus promoting the regeneration and healing of damaged tissues, to achieve the therapeutic purpose of pain relief.
6.1 Laser treatment was added during the operation
Compared with the addition of laser treatment after surgery, the first day was redness, while the redness was more severe in the addition of laser treatment. It can be seen that adding laser treatment can better help reduce swelling and promote the recovery of pets.
6.2 Laser therapy was added after the surgery
Compared with previous cases that have not added laser treatment, laser has obvious effect on the postoperative treatment of TPLO cases, helping pets recover and reduce pain faster. Specifically, the postoperative swelling was fast, the animals were willing to walk on the second day of surgery, and the weight recovery time was earlier.
6.3 Global assessment
Typically, animals undergoing TPLO surgery can regain their normal motor function six to eight weeks after surgery. In this case,laser was used for postoperative recovery treatment, and only two weeks were used to restore the normal walking state, indicating that laser treatment had a good therapeutic effect in promoting tissue healing and relieving pain.
1. Peter Muir, Advances in The Canine Cranial Cruciate LIgament 2th edition, 2018
2. Spencer A. Johnston, Karen M. Tobias, Veterinary Surgery Small Animal 2th edition, 2017
3. Dominique Griffon, Annick Hamaide, Complications in Small Animal Surgery, 2016
4.Laser Therapy in Veterinary Medicine Photobiomodulation,Ronald J. Riegel,John C. Godbold, Jr.