Laser Therapy for Peri-Implantitis
The World Consensus Conference divided periimplant diseases into the following four categories:
1. Health around the implant.
2. Perimplplanimplant mucositis.
3. Peric implantitis.
4. Soft and hard tissue defects around the implant.
The latter three categories belong to the broad category of peri-implantitis. And some studies have reported that the incidence of peri-implantitis is as high as 28.5%.
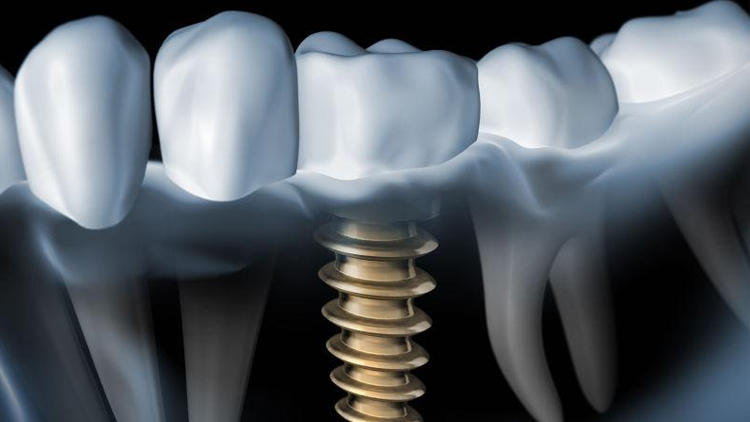
Peri-implantitis is an inflammatory disease occurring in the soft and hard tissue around the implant, which is clinically manifested by different degrees of bone tissue loss, accompanied by the formation of periimplant bags, exploratory bleeding and exploratory pus discharge. Similar to periodontitis, peri-implantitis is caused by the accumulation of peri-implant plaque, which is similar to the subgingival bacterial plaque flora of periodontitis. Peri-implantitis can cause inflammation of the periimplant soft tissue and bone resorption, eventually leading to loosening and shedding of the implant.
The treatment principle of periimplantitis is to remove pathogenic factors, remove plaque, control infection, eliminate periimplant bags, stop bone loss, induce bone regeneration, and restore the original tissue structure.
At present, the treatment methods of peri-implantitis can be roughly divided into non-surgical treatment and surgical treatment. Cases with severe bone resorption and a periimplant exploration depth that is still above 5 mm after routine treatment should be treated surgically. In addition, non-surgical treatment is recommended. Non-surgical treatment means include mechanical debridement, drugs, laser, ozone, hyperbaric oxygen, etc., among which mechanical debridement and plaque removal are the basic treatment measures and the basis of all treatment methods. Meanwhile, drug and laser therapy are two effective non-surgical treatments that are widely used in the clinic.
Diode laser refers to a low-energy laser containing parameters such as certain power, wavelength, pulse length, pulse frequency, pulse duration, total radiation duration, intensity, pulse interval and dose. It has a significant inhibitory effect on the growth of enterococcus faecalis, staphylococcus aureus and glinopromonas gingivalis, and has no damage to the implant. Diode laser can inactivate the LPS attached to titanium discs, inhibit the activation of macrophages, and reduce the number of S. aureus, thus achieving the effect of inhibiting inflammation. Diode laser can affect the survival and proliferation of stromal cells, fibroblasts, and osteoblasts, enhance biocompatibility, and play an active role in peri-implantitis treatment. Diode laser can also enhance local blood circulation, regulate body immunity, accelerate wound healing, reduce inflammatory response, promote cell growth, tissue repair, so as to effectively treat periimplant inflammation. Diode laser treatment of periimplant implantitis not only has a bactericidal effect, but also has a decontamination effect on the implant surface, promoting the formation of biological closure at the interface between the implant and the gum, and is conducive to the periimplant bone integration and bone regeneration.